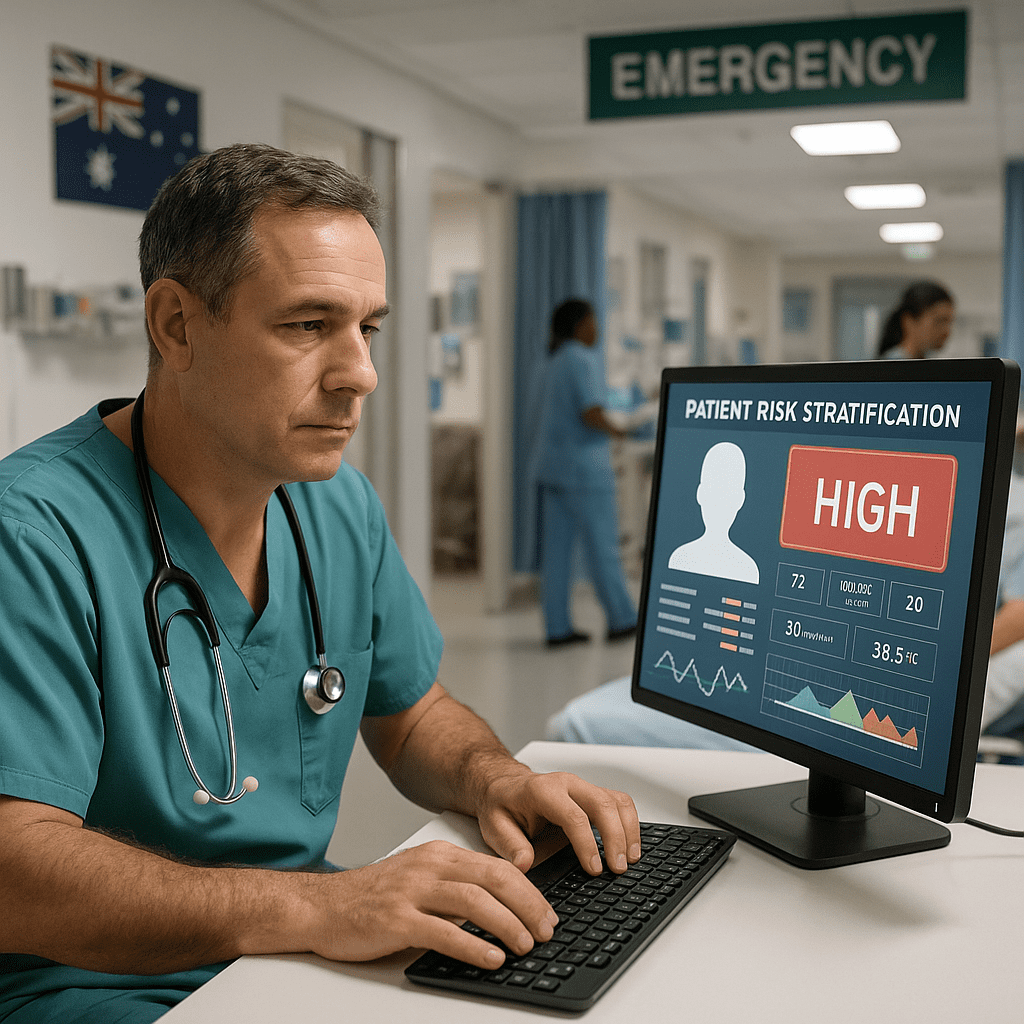
How AI-Powered Risk Stratification Tools Are Improving Patient Triage in Australian Hospitals
Published by SMPLSINNOVATION — Health technology consulting that keeps things smart, simple, and a little bit cheeky.
I. Introduction
Let’s be honest — the waiting room at a busy Australian hospital on a Friday night can feel like a big social event. You’ve got the rugby fan with a dislocated shoulder, the parent trying to calm a worried toddler, and the tired staff working hard to help everyone.
Emergency departments are facing record numbers of patients and continuing staff shortages, according to the Australian Institute of Health and Welfare (AIHW, 2023). But in the middle of all this, something exciting is happening — artificial intelligence (AI) is stepping in to help.
This post looks at how AI-powered risk tools are changing the way hospitals triage patients across Australia in 2024, making care faster, smarter, and fairer.
II. The Current State of Patient Triage in Australia
Waiting times in emergency departments have become a national topic. The AIHW’s 2023 Emergency Department Care Report showed more people coming to hospital across all levels of urgency, with waiting times getting longer in big city hospitals.
Traditional triage depends on nurses using their skills and judgement to decide who needs help first. But this system has some limits:
1. It can be subjective — two nurses might give different urgency levels to the same patient.
2. There is too much data — hospitals collect lots of information, but staff often can’t look through it all quickly.
3. Sometimes signs of serious illness are missed until it’s too late.
That’s why Australia’s National Digital Health Strategy Refresh (2023–2024) is calling for more AI use, better data sharing, and fair access to technology.
III. The Concept of AI-Powered Risk Stratification
Risk stratification means sorting patients based on how sick they are or how sick they might become. It’s like using math instead of magic to look into the future.
AI models can predict things like the risk of needing intensive care, developing sepsis, or being readmitted to hospital.
Common types of models include:
1. Logistic regression — a simple and explainable method.
2. Deep learning — powerful systems that look for patterns in data, like changes in vital signs or images.
3. Ensemble methods — combining several models to get stronger results.
These tools use many different types of data, such as:
Electronic medical records, vital signs, lab results, imaging, wearables, patient surveys, medicine histories, environment and demographic details, clinical notes, and past hospital outcomes.
The more diverse the data, the better the AI can learn — but this also raises privacy concerns. Under the Australian Privacy Principles (APPs), AI systems must protect personal data, keep it safe, and only use it for approved health purposes.
IV. Key AI Tools and Pilot Programs in Australian Hospitals (as of Early 2024)
AI in Australian hospitals is no longer just an idea — it’s happening. Some examples include:
1. CSIRO’s AI Clinical Decision Support System, used to share predictive models in hospitals.
2. St Vincent’s Hospital Sydney, where AI helps spot patient deterioration in real time.
3. Monash Health’s Predictive Deterioration Algorithm, which is showing strong early results.
4. Queensland Health’s Smart Triage Project, which uses AI to manage emergency department flow.
5. Alfred Health’s Sepsis Detection Model, helping identify infections earlier.
6. Royal Adelaide Hospital’s Cardiovascular Risk Tool, built with CSIRO for heart patients.
7. Western Australia Health AI system that connects with the national My Health Record.
8. Northern Health’s AI system that prioritises serious fracture cases.
9. NSW Virtual Care Hub, which uses AI to triage telehealth calls.
10. University of Sydney’s 2024 AI Equity and Bias Audit, which checks fairness in triage tools.
These pilots show that AI isn’t replacing doctors or nurses — it’s helping them do their jobs better.
V. How AI Improves the Patient Triage Process
AI triage tools act like super helpers who never get tired and can pick up tiny clues that a patient is getting worse. They bring many benefits:
1. Faster decision making so high-risk patients are seen sooner.
2. More accurate risk detection using large amounts of data.
3. Consistent triage decisions between staff.
4. Better use of staff and hospital beds.
5. Early signs of illness spotted before it becomes serious.
6. Alerts built directly into hospital systems.
7. A smoother, clearer process that builds patient trust.
8. Useful data to guide hospital planning.
9. Remote triage for telehealth services.
10. Continuous learning so the AI improves over time.
VI. Ethical, Privacy, and Equity Considerations
AI is only as fair as the data it learns from. The University of Sydney’s 2024 study found that some triage tools didn’t perform as well for Indigenous patients and people from lower income areas.
That’s why Australia’s health and digital agencies are setting up strong ethical rules for AI, including:
1. Clear and open systems.
2. A wide mix of data to avoid bias.
3. Testing across different groups.
4. Human oversight at all times.
5. Regular reviews to catch problems early.
Smart technology should support every patient, no matter who they are.
VII. Challenges and Lessons Learned
Even great AI needs updates and real-world testing. Hospitals using these systems have faced some challenges, such as:
1. Difficulties connecting AI with older computer systems.
2. Some staff still preferring their own judgement.
3. Meeting strict privacy and policy rules.
4. Limited budgets.
5. Incomplete or messy data.
6. Cybersecurity risks.
7. Staff feeling tired of constant change.
8. A shortage of AI training for hospital workers.
9. Slow and complex purchasing processes.
10. Long ethical review times before approval.
Despite these hurdles, hospitals using AI triage have seen improvements in efficiency, confidence, and teamwork.
VIII. The Future of AI-Driven Triage in Australia
Australia’s major health and research groups — including CSIRO, the Australian Digital Health Agency, and state health networks — are working together to unify AI standards. By 2025, we can expect:
1. Broader AI use within the My Health Record system.
2. Better data sharing for hospitals across the country.
3. Federated learning models that keep patient data local and secure.
4. AI-based triage in rural and Indigenous communities.
5. National approval and quality checks for AI tools.
6. Dashboards that show real-world outcomes linked to AI accuracy.
With the right guidance and teamwork, AI can help hospitals give faster and fairer care to every Australian patient.