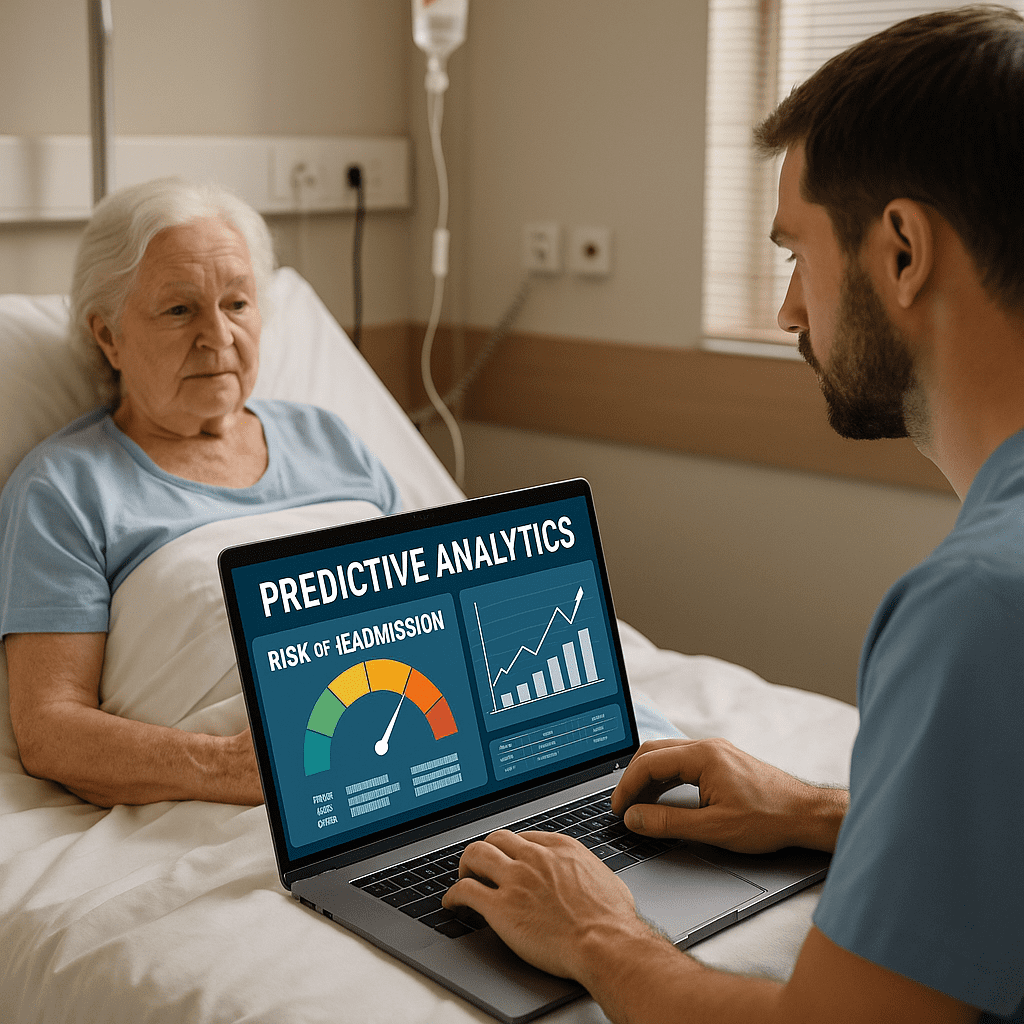
The Role of Predictive Analytics in Preventing Hospital Readmissions for Aged Care Residents
By SMPLSINNOVATION — because keeping Grandma out of the hospital (and on the dance floor) is everyone’s goal.
I. Introduction
You know that feeling when your aged care residents are finally stable, comfortable, and happy after leaving the hospital, and then suddenly their name shows up again on the readmission list? It’s frustrating for everyone on the care team.
Hospital readmissions for older adults are becoming a big challenge in 2024. According to BMJ Health & Care Informatics (Feb 2024), readmission rates for long-term care residents in OECD countries have gone up by 4.7% each year. The main reasons are complex health problems, short staffing, and poor care transitions.
Here’s some good news: predictive analytics is helping doctors and nurses spot problems before they happen. By looking at real-time data and patterns, health teams can find out who is most likely to go back to the hospital and why. The result is fewer ambulance trips, happier residents, and better use of healthcare budgets.
Let’s see how predictive analytics is changing aged care and helping stop unnecessary readmissions.
II. Understanding Hospital Readmissions in Aged Care
1. How Common It Is
– Australia: 30-day readmission rates for aged care residents are around 18–20%, based on 2024 data from the Australian Institute of Health and Welfare.
– United States: JAMA Network Open (Jan 2024) found almost 1 in 5 Medicare residents in aged care have a preventable readmission each year.
– United Kingdom: The Lancet Digital Health (Dec 2023) showed that 23% of care home readmissions were due to poor coordination between care providers.
2. Main Causes
There’s no single cause. It’s usually a mix of issues such as:
– Weakness and injuries from falls.
– Taking too many medications.
– Having many chronic illnesses at once.
– Poor transitions from hospital to home.
– Lack of family or community support.
– Delays in follow-up visits after discharge.
3. How It Is Measured
Healthcare workers track readmissions using:
– 30-day readmission rate: The percent of residents who return to hospital within a month.
– Potentially Preventable Readmission (PPR): Cases that could have been avoided with better care.
– Unplanned admissions: Emergency returns without scheduled follow-up.
4. New Evidence
A 2024 study in Frontiers in Digital Health found that using predictive models with team-based follow-up reduced unplanned hospital visits by 12–18%. The best results came from combining smart analytics with active human care.
III. Basics of Predictive Analytics in Healthcare
Predictive analytics uses math, data, and computer systems to guess what might happen next. For example, it can predict if someone might need to go back to the hospital soon. Prescriptive analytics takes it a step further and helps decide what actions to take to stop that from happening. Think of predictive analytics as the crystal ball, and prescriptive analytics as the smart advisor.
Data that powers predictive analytics includes:
– Electronic Health Records (EHRs) with medical histories.
– Remote patient monitoring with daily vital signs.
– Wearable devices like smartwatches and fall sensors.
– Social factors, like loneliness or lack of support.
– Clinical notes and images from doctors.
Popular models include logistic regression, gradient boosting, random forests, deep neural networks, and federated learning, which protects privacy by not sharing personal data directly.
These models are checked for accuracy using tests like AUROC scores, precision and recall, and explainability tools that help doctors understand why a patient was flagged as high risk.
IV. Top 10 Ways Predictive Analytics Helps Stop Readmissions
1. Risk scoring tools inside EHRs that flag residents at risk.
2. Early warning alerts from continuous monitoring.
3. Detecting when medication schedules are not followed.
4. Finding signs of social isolation or loneliness.
5. Alerts for residents who need extra care when leaving the hospital.
6. Virtual follow-up care after discharge using telehealth.
7. Tracking diet and hydration to prevent dehydration.
8. Predicting falls using motion sensors and gait data.
9. Checking whether therapy programs are followed properly.
10. Shared dashboards to help teams coordinate care.
A 2024 Health Affairs report found that aged care facilities using five or more predictive tools saw double-digit drops in readmissions, proving that teamwork and technology together work best.
V. Real Examples and Studies
1. In Australia, an aged care group used an AI Health Dashboard in 60 facilities. It gave nurses early risk alerts and reduced 30-day readmissions by 15.2% in six months. The key was that the system explained its predictions clearly, so staff trusted it.
2. In Europe, a study using federated learning across five elder-care networks predicted readmissions without sharing private patient information. Accuracy improved by 9%, showing that privacy and performance can go hand in hand.
3. In the United States, a housing network in New York used predictive tools to track residents’ blood pressure and medication use after discharge. Nurses acted within 48 hours to prevent serious issues.
4. In Japan, predictive models helped spot dehydration and poor nutrition in older adults, cutting readmissions by 12%.
5. In Nordic countries, cross-facility AI dashboards helped care teams share information and reduced emergency transfers by 10%.
VI. Challenges and Things to Work On
Predictive analytics has huge promise, but it’s not perfect. Some of the main challenges include:
– Protecting personal data and following privacy laws.
– Avoiding bias and unfair predictions.
– Keeping models updated as health trends change.
– Training clinicians so they can trust and use the tools.
– Making new systems work well with older ones.
– Handling the cost of new technology.
Predictive analytics is not magic, but with the right balance of technology, teamwork, and care, it can help older adults stay healthier and spend more time enjoying life instead of returning to the hospital.